
TTUHSC’s new vision — transform health care through innovation and collaboration — ideates a community of diverse individuals empowered to effect change through ingenuity and teamwork.
Without you, we wouldn’t be where we are today, and we’re excited about your role in our future. The future of health care.

In our technologically driven environment, operating without internet access is like trying to breathe without oxygen — you flatline. What transpired over the next 48 hours, however, was nothing short of a miracle. In a project that should have taken two weeks, competitive vendors worked together to restore internet accessibility in two days. Our chief information officer and vice president of information technology, Vince Fell, called it a “case study in teamwork.”
We’re honored to share the story in this issue about our ninth president. Lori Rice-Spearman, PhD, (Health Professions ’86) worked her way from student to our university’s helm. She is leading TTUHSC with a new vision: transform health care through innovation and collaboration.
You will notice the “Innovation & Collaboration” logo on certain stories throughout this and our summer 2021 issues. We are labeling stories that directly coincide with the new vision and hope you will find inspiration in the creative and interprofessional work done by our faculty, staff and students.
Best wishes for health and happiness this coming year.
Office of External Relations
Excerpt from the summer 1990 issue
It was about 16 hours before we had resumption of lab facilities — a hardship for me since I had four fresh heart surgery patients to care for. We all survived, but I ended up having to stay in the hospital for four straight days (and nights) while we tried to stabilize/transfer/sort out things.
Actually, I had made plans before the quake to relocate. I have left general surgery at Stanford to do emergency medicine in Denver, and I love it. This is a very dynamic program, and I feel like I’ve finally started learning in a residency. Denver is great, and the people are more like Texans, (but don’t tell them I said that!) so I just feel like I’m home.
SCL Health System
TTUHSC School of Nursing

ttuhsc School of Medicine
Covid patients in the hospital being isolated, alone, sick, and afraid. Those dying are doing it alone via FaceTime. How terrible is this!!!!
Danette Baker, MA
Kara Bishop
Jim Nissen
Davide Bonazzi, Ivan Canu, Suzanna Cisneros, Carolyn Cruz, East Carolina University, Norman Drew, Neal Hinkle, Kami Hunt, Sarah Lyons, Angie McCue, Cameron Onks, JD, Jordan Pape, Melissa Whitfield, Glenys Young
Lori Rice-Spearman, PhD
(Health Professions ‘86)
Ashley Hamm
Mattie Been, Amarillo
Jessica Zuniga, Permian Basin
Cyndy Morris
Kevin Friemel, Smiley Garcia, Kendalyn Rising, Clifford Wilkes
pulse@ttuhsc.edu
TTUHSC External Relations
3601 Fourth Street 6242 6238
Lubbock, TX 79430-6238
Bachelor of Science in Clinical Laboratory Science
Second Degree Bachelor of Science in Clinical Laboratory Science
Post-Bavvalaureate Certificate in Clinical Laboratory Science
Master of Science in Molecular Pathology
Master of Physician Assistant Studies
Rehabilitation Sciences
Master of Athletic Training
Master of Occupational Therapy
Doctor of Occupational Therapy
Post-Professional Doctor of Occupational Therapy
Doctor of Physical Therapy
Doctor of Science in Physical Therapy
Doctor of Philosophy in Rehabilitation Science
Concentration in Communication Sciences Disorder
Concentration in Movement Sciences Disorder
Speech, Language & Hearing Sciences
Doctor of Audiology
Bachelor of Science in Speech, Language, and Hearing Sciences
Second Degree Bachelor of Science in Speech, Language, and Hearing Sciences
Master if Science in Speech-Language Pathology
Healthcare Management & Leadership
Bachelor of Science in Healthcare Management
Master of Science in Healthcare Administration
Graduate Certificate in Health Informatics and Data Analysis
Graduate Certificate in Health Systems Policy and Management
Graduate Certificate in Healthcare Finance and Economics
Graduate Certificate in Health Systems Engineering and Management
Graduate Certificate in Long Term Care Administration
Clinical Counseling & Mental Health
Master of Science in Addiction Counseling
Master of Science in Clinical Mental Health Counseling
Master of Science in Clinical Rehabilitation Counseling

Bachelor of Science in Clinical Laboratory Science
Second Degree Bachelor of Science in Clinical Laboratory Science
Post-Bavvalaureate Certificate in Clinical Laboratory Science
Master of Science in Molecular Pathology
Master of Physician Assistant Studies
Rehabilitation Sciences
Master of Athletic Training
Master of Occupational Therapy
Doctor of Occupational Therapy
Post-Professional Doctor of Occupational Therapy
Doctor of Physical Therapy
Doctor of Science in Physical Therapy
Doctor of Philosophy in Rehabilitation Science
Concentration in Communication Sciences Disorder
Concentration in Movement Sciences Disorder
Speech, Language & Hearing Sciences
Doctor of Audiology
Bachelor of Science in Speech, Language, and Hearing Sciences
Second Degree Bachelor of Science in Speech, Language, and Hearing Sciences
Master if Science in Speech-Language Pathology
Healthcare Management & Leadership
Bachelor of Science in Healthcare Management
Master of Science in Healthcare Administration
Graduate Certificate in Health Informatics and Data Analysis
Graduate Certificate in Health Systems Policy and Management
Graduate Certificate in Healthcare Finance and Economics
Graduate Certificate in Health Systems Engineering and Management
Graduate Certificate in Long Term Care Administration
Clinical Counseling & Mental Health
Master of Science in Addiction Counseling
Master of Science in Clinical Mental Health Counseling
Master of Science in Clinical Rehabilitation Counseling

At TTUHSC, however, it was anatomy as usual thanks to expanded facilities in the new Institute of Anatomical Sciences’ gross anatomy lab.
“It’s difficult to grasp a 3D perspective on a two-dimensional screen, so we’re grateful that we had the opportunity to safely provide practical instruction for our students,” said Kerry Gilbert, PT, ScD, (Health Professions ’04, ’97) co-director of the institute.
COVID-19 delayed the official opening of the 20,000 square-foot lab until December, but the space was completed in time for use by incoming students in health professions, medicine and biomedical sciences. The facility allowed for the necessary physical distancing, enabling university leadership to approve in-person instruction.
 Breaking Barriers
Breaking Barriers
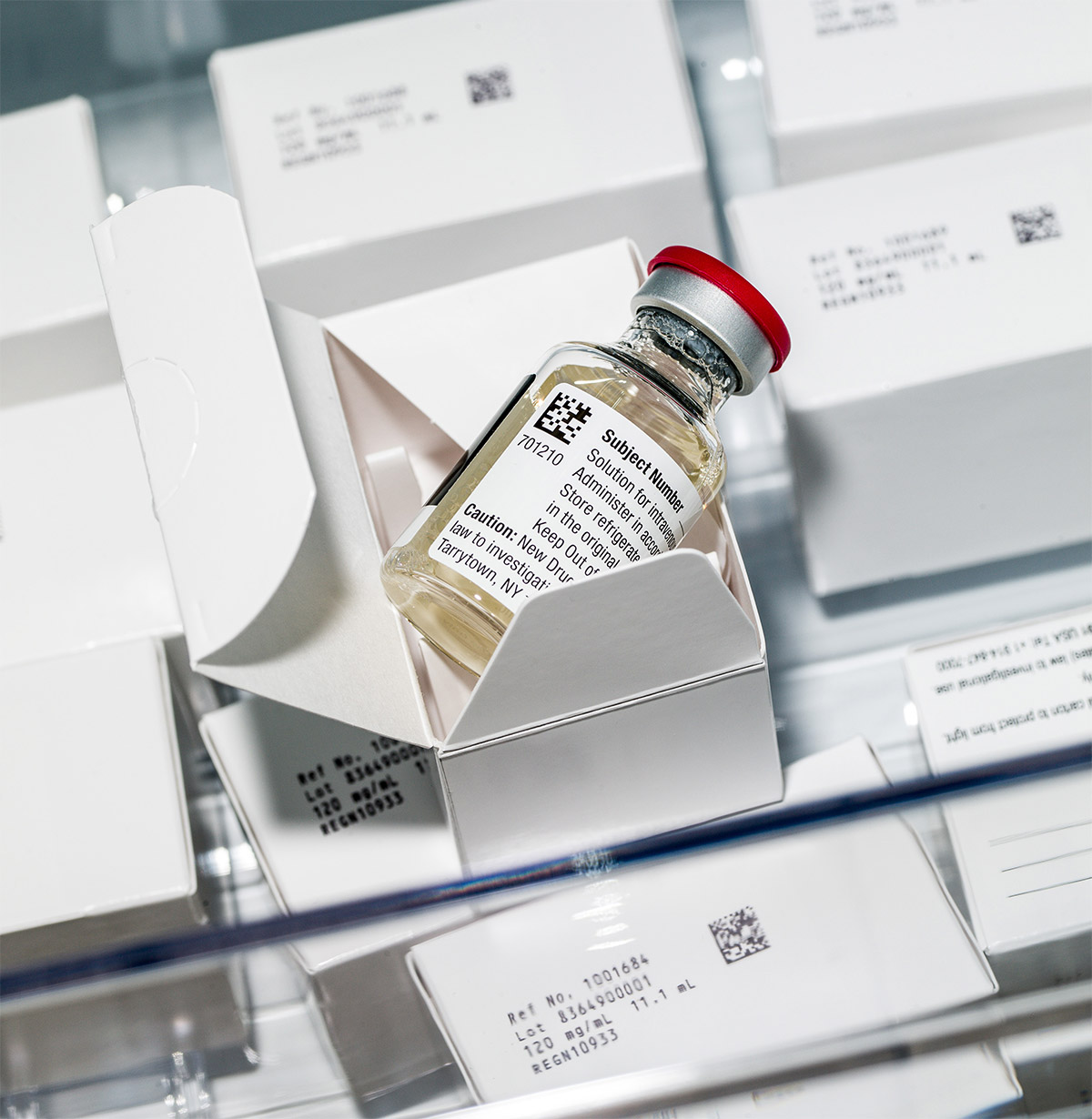
“We could not pass up the opportunity to be a part of this effort,” said Sigler, assistant professor in the School of Medicine Department of Internal Medicine in Amarillo. “This company made the best treatment for the Ebola virus, and they’re giving West Texas the opportunity to participate.”
Sigler reached out to PharmaTex Research LLC, an Amarillo-based research and product development company who agreed to assist with the trial. As of press time, TTUHSC Amarillo has enrolled 220 patients in the trial for Regeneron’s potential COVID-19 treatment. On Nov. 21, 2020, Regeneron was issued an emergency use authorization from the Food and Drug Administration due to positive results from the ongoing trial.
in Texas
Why is this procedure important for West Texas?
It puts patients’ needs first.
Some patients are classified as high risk for surgery because they have other conditions, like obesity, age or history of smoking, that can complicate the procedure or anticipated recovery. This procedure provides an option for those denied traditional surgery.
It combats stereotypes.
“West Texas is kind of ignored, and all of these new techniques and new interventions usually go to the bigger cities of Dallas and Houston,” said Ansari, cardiology assistant professor in the School of Medicine. “So, it was awesome for me not only to help my patient, but also to tell everybody in Texas, ‘We in Lubbock can perform these procedures and help our patients exactly like everyone else.’”
It’s life-changing.
Ansari says when patients come into the hospital for the surgery, they’re usually in severe pain and unable to walk. “You can see the difference the next day,” he said. “When they come to the clinic to follow up, they say, ‘I am back to mowing my lawn. This was something I never dreamed I would be able to do again.’”
 FACULTY PROFILE
FACULTY PROFILEProfessor, Graduate School of Biomedical Sciences
Bryan Sutton, PhD, divides his work time between writing papers and grants, grading student assignments and overseeing their research projects examining the role of proteins in muscular dystrophy. Outside of work he’s developed a well-rounded life perspective from his curious nature. While he’s not a “Sound of Music” junkie, he does have a list of his favorite things.
Favorite Movie: Star Wars
I still remember watching it for the very first time when I was 12 years old.
Favorite instrument: Scottish Bag Pipes
While in college, I saw a group play the bag pipes. I enjoy watching how things work, and the mechanics of the instrument fascinated me. They taught me how to play, and I’ve been hooked ever since — even though I’m not Scottish.
Favorite season: Summer
I don’t like the cold, which may be why when I moved from North Carolina to Texas, I stayed. It’s been three decades now.
Favorite experience: Mount Everest
Michael Blanton, PhD, (professor in the School of Medicine) manages a faculty hiking club and set up a TTUHSC expedition to Mount Everest. I went to the south base camp in Nepal in October 2019 with Blanton and Thomas Pressley, PhD, also a professor in the School of Medicine. While I don’t remember it being bitterly cold, I do remember the lack of oxygen and rocky terrain. We hiked 40 miles from Lukla, Nepal, to base camp, averaging 10 miles per day. With an altitude of 17,598 feet at base camp, it’s hard to sleep, and you have no appetite. It was a difficult but fun trip surrounded by things you wouldn’t see in Lubbock, Texas. This planet is a really beautiful place.

 for the record
for the record
“We once received an old-fashioned alarm clock at the Medication Cleanout once.”
MANAGING DIRECTOR, TEXAS PANHANDLE POISON CENTER



Let’s unpack the box.
BlueGel Electrophoresis System with Integrated Illuminator:
This machine, with a built-in blue light transilluminator can visualize DNA as it separates, seeing bands in as little as five minutes.
MiniPCR Mini8 Thermal Cycler:
This portable polymerase chain reaction (PCR) machine has an eight-well capacity and can be operated through computers, smartphones and tablets. It’s used to perform PCR, which is an important step in analyzing DNA.
Micropipettes:
The kit comes with three sets, in different volumes, of this quintessential biotech tool.

Let’s unpack the box.

1
BlueGel Electrophoresis System with Integrated Illuminator:
This machine, with a built-in blue light transilluminator can visualize DNA as it separates, seeing bands in as little as five minutes.
2
MiniPCR Mini8 Thermal Cycler:
This portable polymerase chain reaction (PCR) machine has an eight-well capacity and can be operated through computers, smartphones and tablets. It’s used to perform PCR, which is an important step in analyzing DNA.
3
Micropipettes:
The kit comes with three sets, in different volumes, of this quintessential biotech tool.
 School of Health Professions
School of Health Professions10-foot view:
In the first step of his research, Thompson needs to validate the utility of ultrasound as a measurement tool here on earth, before it can be used to measure spinal health in space. Initial studies in this area used MRI machines, which aren’t compatible with long-term spaceflight. “It’s more cost effective than MRI equipment, and it’s the only equipment that can fit in the training shuttle so we can measure the pressure put on the spine in space.”
30,000-foot view:
This research shows potential as a tool for developing treatment options for chronic neck pain. A 2010 Global Burden of Disease study identified neck pain as the fourth highest in terms of years lived with disability, validating the necessity of preventive treatment.
1,000,000-foot view:
Measurements of the cervical spine in space could provide information to help prevent spinal degeneration in astronauts when they travel to the moon or ever take a trip to Mars. “It’s only every 18 months that the Earth and Mars are in alignment where you can even send an astronaut there to work and bring him or her back,” Thompson said. “So how do we prevent cervical injury during a long-term mission in space?”

 School of Health Professions
School of Health Professions As a TTUHSC audiology student, Ortiz met Joseph Pratt, AuD, CCC-A, (Health Professions ’13). They quickly bonded over their shared goal of military service. After earning their doctorate degrees, both men were commissioned as audiologists in the U.S. Navy.
As clinical audiologists, a significant aspect of their job was hearing conservation, a practice area that attracts only 5% of audiologists. After seeing 18- and 19-year-olds with life-altering hearing loss, Ortiz and Pratt became even more passionate about auditory preservation.
 SCHOOL OF NURSING
SCHOOL OF NURSINGHospital fire.
Mass shooting.
Global pandemic.
Brandon “Kit” Bredimus, DNP, RN, (Nursing ’19, ’15) had a memorable first year as the vice president of nursing and chief nursing officer for Midland Memorial Hospital in Midland, Texas. He’s used to rolling with the punches and taking criticism in stride. Family members said he’d make a terrible nurse. Two days after he was named CNO, a hospital surveyor reported Bredimus lacked experience for the position. He never stopped working and now, not only is he an accomplished nurse, he also has led the hospital’s nursing staff through three significant disasters — all in the same year.
“Nursing is both a science and an art,” Bredimus said. “It’s a beautiful thing to address the technical side of health care without losing your humanity. That’s what I strive to do every day.”
(Nursing ’19, ’15)

On Aug. 6, 2020, the Texas Tech University System Board of Regents approved the creation of a fully online MSN-MBA dual-degree program. Students and faculty provide their top reasons for pursuing this degree.
1 | No Duplication
Some courses in the MSN program are accepted by the MBA program. “I received my MSN this past year, so now I only have 18 months to go to get my MBA instead of three years,” said Amanda Griswold, MSN, BSN, RN, (Nursing ’20, ’17) chief nursing officer for McCamey County Hospital District in McCamey, Texas, and a student in the dual-degree program.
2 | Ready for Leadership Roles
Audra Ellis, BSN, RN, (Nursing ’16) nursing manager of the staffing operations unit for Covenant Health, aims to enhance her skills through the program. “I think understanding the financial side of health care will be beneficial, not only for me to understand the bigger picture of hospital administration but to also communicate business decisions to my nursing staff effectively,” she added.
3 | Build Confidence as a Nurse
“As health care professionals serving on the front lines every day, no one understands resource conservation like a nurse,” said Cindy Acton, DNP, MSN, RN. She and Barbara Cherry, DNSc, MBA, MSN, RN, (Nursing ’97) created thi program for nurses interested in extending their business skills following the launch of TTU Rawls College of Business’ accelerated online MBA degree. This program equips nurses with tools needed to lead in their field and to effect policy change for the benefit of the health care system.
 SCHOOL OF NURSING
SCHOOL OF NURSING
As she prepares for her training evaluation, level-two nursing student Laura Haffner strategically drapes clothes from her closet onto pillows, creating a “patient.” COVID-19 prevented students from training in The F. Marie Hall SimLife Center in Lubbock; and, as they have in every aspect of their lives since the pandemic hit, Haffner and nursing students across the university adapted.
“It was pretty strange to be conducting an examination on my pillows, but I got the job done,” Haffner said, adding with a laugh, “some of my classmates even had emoji pillows that gave ‘faces’ to their patients.”
Simulation training creates the most realistic environment possible to provide an optimal training experience for students. TTUHSC faculty identified obstacles of teaching technical skills online and a need for better remote training, which led to the new Modular Skills Trainer, or “Sim-in-a-Box.” Team members from TTUHSC’s Simulation Program assisted the vendor in designing the skills trainer.
TTUHSC was the only university selected for product beta testing. Haffner was one of 90 nursing students across multiple campuses chosen to work with the training model and provide input on its design. The portable simulation tool is a 5” by 9” cardboard box with attachments allowing students to practice skills such as inserting urinary catheters, performing wound care and practicing IV starts.



Permian Basin
 Jerry H. Hodge School of Pharmacy
Jerry H. Hodge School of PharmacyThe dangers of substance use disorder from prescriptions have been making headlines for 30 years since the first cases of opioid addiction in the 1990s. But over-the-counter medications (OTC) shouldn’t be overlooked as they carry similar risks.
Some people incorrectly assume medications are safe if they don’t require a prescription, particularly adolescents and teens — the most vulnerable populations to addiction. To reduce the risk, buy OTCs in small quantities, recommends Jeanie Jaramillo-Stametz, PharmD, (Pharmacy ’01) managing director of the Texas Panhandle Poison Center and assistant professor in the Department of Pharmacy Practice.


(Pharmacy ’01)
Managing director, Texas Panhandle Poison center

 Jerry H. Hodge School of Pharmacy
Jerry H. Hodge School of Pharmacy
“This study shows that in three years you can more than pay for the program,” said Charles F. Seifert, PharmD, FCCP, BCPS, pharmacy regional dean in Lubbock and co-principal investigator. “What I would like to see is hospitals and other health care institutions, taking the model and utilizing it to improve patient care. I think if the population is selected correctly it can be beneficial in any situation.”


Antimicrobial Stewardship Pharmacist
Northwest Healthcare System
Amarillo, Texas

Owner/Consultant Pharmacist
Manage Meds LLC
Sulphur Springs, Texas
BRAKEBILL: I look at all the antibiotics and round with doctors. Twenty years ago, we were in the basement verifying orders; you would not have seen us on the hospital floor suggesting medications.
Why should pharmacists be involved in treatment processes?
WHITE: Pharmacists advocate for patients, so they can be on the least amount of effective medications possible. Sometimes the medications are no longer viable or cause complications when used as a long-term treatment option.
How is a pharmacist/physician partnership beneficial?
BRAKEBILL: Patient needs fall into one of two categories: pharmacokinetics and pharmacodynamics. There is a reciprocal relationship between the drugs and the body. Pharmacists help physicians tailor medication to the individual.
How can pharmacists help with provider shortages?
WHITE: Collaborative practice between pharmacists, physicians, nurse practitioners, physician assistants, etc., is very important. We’re even seeing pharmacists advocating for a role in COVID-19 testing. There are a lot of things that pharmacists can help with so physicians can spend more time with their patients — medication therapy management is one example. There is even more opportunity for collaborative partnerships in rural areas, due to high demand for providers.
 graduate school of biomedical sciences
graduate school of biomedical sciences
So, disease prevention became his primary focus, leading Appiah on a quest beyond clinical practice. He earned a master’s of public health and doctorate in epidemiology from the University of Louisville. Appiah’s research took a detour through cardiovascular disease, but came full circle when one of his students approached him with a potential research project.
 SCHOOL OF MEDICINE
SCHOOL OF MEDICINE
 SCHOOL OF MEDICINE
SCHOOL OF MEDICINE

Lori Rice-Spearman, PhD
(Health Professions ’86)
President
Perfect
Storm
Cameron Onks, JD
Director, F. Marie Hall Institute for Rural and Community Health Innovative Healthcare Technology Excerpts from “COVID-19: Telemedicine’s Perfect Storm” published in Rural Health Quarterly Magazine, May 2020.
Danette Baker, MA
Editor, Pulse
Excerpts from “Remote Access” published in Pulse, Summer 2000.

anuel and Maria Porras became proud parents on a Friday afternoon in June of a beautiful daughter they named Aida. Maria had dreamt of the moment when she would hold her baby for the first time, but instead a nurse took the baby away immediately after birth. “I waited for them to bring her back, but instead they told me she was really sick.”
James Luecke, MD, a family medicine physician at Big Bend Regional Medical Center in Alpine, Texas, successfully delivered the Porras’ healthy baby girl on June 29, 1990, but within minutes, his tiny patient was in respiratory distress. In fact, Luecke had moved to his next case — a surgical telemedicine consult — when he learned about Aida’s condition. Luecke asked the surgeon online if there was a neonatologist available in Lubbock for an emergency consult — putting TTUHSC’s fledgling telemedicine program to the test.
Presidential Distinguished Alumni Award


Kenneth D. Cole, PhD (’81)
Sixtus Atabong, MPAS, PA-C (’05, ’02)
Ram Haddas, PhD (’13)
Courtney Sherman, DNP, MHA, MPH
(Health Professions ’17, Nursing ’15)
Bobbie Kay Turkett, MS, CCC-SLP
(’05, ’03)
Justin Berk, MD, MPH, MBA (’15)
Ebtesam Attaya Islam, MD, PhD (Medicine ’09; Biomedical Sciences ’05)
Debra Danforth, DNP (’19)
Christa de la Garza, MSN, BSN, RN (’19, ’16)
Tanna Nelson, MSN, RN-BC, CPHIMS (’15)
Patrick “Race” Dulin, PharmD (’07)
To nominate someone for a distinguished alumni award, visit: ttuhsc.edu/alumni
 SERVING THE SERVICE
SERVING THE SERVICE
School of Nursing — Veteran to Bachelor of Science in Nursing (applies military service toward academic credits).
School of Health Professions — Graduate Certificate in Veteran Services (curriculum designed for competent practice in working with veterans).
 ALL IN THE FAMILY
ALL IN THE FAMILY

(2020)
Election Gold Humanism Society (2015)
Texas Medical Association C. Frank Webber Award (2013)
Boston University Distinguished
Alumni Award (2012)
American College of Physicians
Tennessee Laureate Award (1998)
Award (2020)
The Johns Hopkins Hospital Idoreyin P. Montague MD Community Action Award (2018)
Texas Medical Association Student of the Year (2013)
U.S. Public Health Service Excellence in
Public Health Award (2012)
American Medical Association Foundation Excellence
in Medicine Leadership Award (2012)

CERTIFICATIONS
Election Gold Humanism Society (2015)
Texas Medical Association C. Frank Webber Award (2013)
Boston University Distinguished Alumni Award (2012)
American College of Physicians Tennessee Laureate Award (1998)

CERTIFICATIONS
(sitting for Addiction Medicine boards this year)
The Johns Hopkins Hospital Idoreyin P. Montague MD Community Action Award (2018)
Texas Medical Association Student of the Year (2013)
U.S. Public Health Service Excellence in Public Health Award (2012)
American Medical Association Foundation Excellence in Medicine Leadership Award (2012)





Internal Medicine Residency: 2013
“What do you want to be when you grow up?” It’s a seemingly simple question asked of children that usually ends up a fleeting thought. For Nagendra Gupta, MD, FACP, CPE, it was an answer that would last a lifetime. As a child, he wanted to be a doctor, and as the years passed, Gupta realized the substantial impact he could make on a person’s life by nurturing them back to health. The more the realization dawned on him, the more his passion grew into a lifelong calling.
Today, Gupta directs the hospitalist program at Texas Health Arlington Memorial Hospital.
At the 369-bed facility, he leads a team of over 20 physicians who handle more than 5,000 inpatient encounters each month. His team has implemented hospital initiatives addressing inefficiencies across the board, such as reduced length of stay, decreased readmission rates and improvements in clinical documentation. His leadership is not only transformative but also a reminder that a childhood dream can improve the health and lives of thousands.
— Jordan Pape
 News & Notes
News & Notes
Pharmacy Graduate: 2019
Michael Dean, PharmD, walks into the infusion room at Texas Oncology in Fort Worth, Texas, and kneels beside a patient receiving a chemotherapy infusion. Addressing patient concerns and questions about medication side effects and alternate therapies is rewarding, Dean says.
“Cancer is a terrible disease. I will do everything I can to help them overcome it.”
As a third-year pharmacy student, there wasn’t a hospital rotation available locally in intravenous admixtures for Dean’s degree requirement. TTUHSC arranged a clinical rotation for Dean at Texas Oncology — a circumstance that led to a permanent career.
While there, Dean discovered his calling in oncology. He reviews patient charts throughout the day, oversees dosages in the patient care process, manages patient retail prescriptions and evaluates patient regimens prescribed by physicians.
“We are partners with physicians here, and that feeling of being part of the medical team is awesome.” — Kara Bishop
 News & Notes
News & Notes
Vadivel Ganapathy, PhD,
chair of the Department of Cell Biology and Biochemistry, has been included in the latest edition of the Google Scholar Database as one of the world’s most cited researchers in history.
Monish Makena, PhD, (’17, ’11)
was awarded a 2019-2020 American Association for Cancer Research Fellowship.

Julie Bruce, DPT, (’08, ’02, ’95)
was promoted to outpatient manager at University Medical Center Team Rehab in Lubbock.
Jeramy Davies, MLS, (ASCP)CM, (’11)
joined the Minneapolis VA Health Care System laboratory in Minneapolis, Minnesota, as a medical technologist.
 News & Notes
News & NotesCaprock Alliance for Mental Wellness, Telehealth
Nursing Graduate: 2018, 2014
When Stacy Hobbs starts talking about the difficulties in accessing mental health services, her voice, ordinarily calm, tightens. She exhales sharply, “It’s so frustrating.” But she is working to change that.
A stint at the San Angelo State School introduced Hobbs to patients with developmental disabilities and psychiatric disorders. Years working in hospital emergency rooms showed her how many patients face psychiatric disorders and substance use issues.

Hobbs opened her own practice in July; her work is in high demand now that systemic mental health needs are aggravated by the coronavirus pandemic. Anxiety and depression are on the rise, and slashed treatment facility capacities exacerbate the situation.
“Think about people who are homicidal, suicidal or their bipolar mania is extreme. Only half of those people are able to get the help they need [through in-patient facilities],” Hobbs said. To help bridge the gap, Hobbs now offers telehealth services to patients throughout the state. As her practice grows, so does her impact. — Glenys Young
 News & Notes
News & Notes
Biomedical Sciences Graduate: 1981
After attending college in the Northeast, Robert Lust, PhD, landed at TTUHSC. A school with an all-hands-on-deck atmosphere meant significant overlap in training doctoral and medical students — the only silos he found were in surrounding fields. Lust completed his doctorate and postdoctoral training and took his first faculty position as a research scientist in cardiology at TTUHSC.
When he left TTUHSC in 1986, Lust thought he’d never again find that unique mix of collaboration. And then, a cardiac surgeon at East Carolina University needed a scientist.
“I’m now again in a brand-new medical school. This guy is building a heart surgery research program, and I thought, ‘I’ve been in this world.’
“I had so much exposure to clinical translational research at TTUHSC. They were attracted to a scientist not afraid to go on hospital rounds or into an operating room. That’s exactly what I was trained to do.” The 2002 Distinguished Alumni honoree now trains the next generation. — Glenys Young
 News & Notes
News & NotesHealth Professions Graduate: 2019
Christy Copeland, LPCA, MS, has always been the person others come to with their problems. Eventually, she decided to make a career out of it. But while working through the Clinical Mental Health Counseling program, she learned something about herself:
“Naturally, I’m a fixer,” she said. She had to learn to switch from fixing to listening. To empower and equip her patients to fix their own problems versus doing it for them.

“Fixing the problem for the client takes away their power to choose and takes away their voice,” she explained. “My intern supervisor once told me that we are supposed to work ourselves out of a job — we give our clients the tools to stand on their own so they become independent.”
After passing the National Counselor Exam in August, Copeland is now working toward the 3,000 counseling hours necessary to become a licensed professional counselor. Her goal is to open her own private practice and help many more people stand on their own. — Glenys Young
 Tribute to Juan Fitz, MD
Tribute to Juan Fitz, MDJuan Fitz, MD, (Medicine ’86) clinical professor in the TTUHSC School of Medicine and physician for Covenant Health, died Nov. 3, 2020, of COVID-19 after contracting the disease from a patient. He was an exemplary emergency room physician, a highly respected colleague and a leader in the Lubbock County Medical Society (LCMS), the Texas College of Emergency Physicians and the Texas Medical Association.
To those who knew him at the School of Medicine, he was an inspiring teacher of our medical students for more than a decade. Juan loved being a physician and was as excited about emergency medicine as the day he started as an intern in Michigan. His incredible fiery passion for the emergency room (ER) spread to our students working with him in Covenant Health System ER rotations. The increasing percentage of students at TTUHSC interested in emergency medicine can be attributed to Juan more than any single physician.
I can say with certainty that I never met Juan at any event when he did not ask about when we would have an emergency medicine residency program. How ironic that he died during the year that our emergency medicine residency began. The residency program was established at UMC, and not Covenant, nevertheless Juan’s advocacy was instrumental in the push for this program. Many of the faculty now teaching the current emergency medicine residents had their initial ER experience with Dr. Fitz.
The School of Medicine and the Lubbock County Medical Society Foundation are raising funds for the establishment of an endowed scholarship in Dr. Fitz’s name — a name that will always be associated with excellence in emergency room care in West Texas.
— Steven L. Berk, MD, dean, School of Medicine
After Wade Graham, MD, graduated from the School of Medicine and finished his ophthalmology residency, he joined the faculty of his alma mater to guide others through the process. As an assistant professor and director of the ophthalmology residency program, Graham saw firsthand the struggles residents faced — the professional problems as well as the personal ones.
Today, he partners with two other alum in private practice. Their practice, Thurmond Eye Associates, has been a successful one. So, when the three men decided they were in a position to help current ophthalmology residents, they did. In 2017, Graham (Resident ’99; Medicine ’95), K.C. Bentley, MD, (Resident ’11; Medicine ’07) and Joel George, MD, (Resident ’07; Medicine ’03) began to give $10,000 annually to the Department of Ophthalmology and Visual Sciences. Their gift in October 2020 brought their total giving amount to $40,000.
“We all felt well prepared for our careers and grateful for the education and training we received,” Graham said. “And we thought, what better way to pay it forward than to contribute to the institution that made it possible?”
After Wade Graham, MD, graduated from the School of Medicine and finished his ophthalmology residency, he joined the faculty of his alma mater to guide others through the process. As an assistant professor and director of the ophthalmology residency program, Graham saw firsthand the struggles residents faced — the professional problems as well as the personal ones.
Today, he partners with two other alum in private practice. Their practice, Thurmond Eye Associates, has been a successful one. So, when the three men decided they were in a position to help current ophthalmology residents, they did. In 2017, Graham (Resident ’99; Medicine ’95), K.C. Bentley, MD, (Resident ’11; Medicine ’07) and Joel George, MD, (Resident ’07; Medicine ’03) began to give $10,000 annually to the Department of Ophthalmology and Visual Sciences. Their gift in October 2020 brought their total giving amount to $40,000.
“We all felt well prepared for our careers and grateful for the education and training we received,” Graham said. “And we thought, what better way to pay it forward than to contribute to the institution that made it possible?”

pulse@ttuhsc.edu

That’s why the couple chose to make a Gift of Impact through their estate to establish endowed scholarships at TTUHSC.
Contact Nathan Rice at giftplanning@ttu.edu or 806.742.1781 to discuss your area of impact and how to make a gift.
Contact Nathan Rice at giftplanning@ttu.edu or 806.742.1781 to discuss your area of impact and how to make a gift.


That’s why the couple chose to make a Gift of Impact through their estate to establish endowed scholarships at TTUHSC.
Scholarships help students pay education expenses but can also impact their career, Jumper said. With less debt to repay, a student’s employment options broaden, allowing them to consider areas of impact rather than debt repayment.
Contact Nathan Rice at giftplanning@ttu.edu or 806.742.1781 to discuss your area of impact and how to make a gift.