Perfect
Storm
Cameron Onks, JD
Director, F. Marie Hall Institute for Rural and Community Health Innovative Healthcare Technology Excerpts from “COVID-19: Telemedicine’s Perfect Storm” published in Rural Health Quarterly Magazine, May 2020.
Danette Baker, MA
Editor, Pulse
Excerpts from “Remote Access” published in Pulse, Summer 2000.

anuel and Maria Porras became proud parents on a Friday afternoon in June of a beautiful daughter they named Aida. Maria had dreamt of the moment when she would hold her baby for the first time, but instead a nurse took the baby away immediately after birth. “I waited for them to bring her back, but instead they told me she was really sick.”
James Luecke, MD, a family medicine physician at Big Bend Regional Medical Center in Alpine, Texas, successfully delivered the Porras’ healthy baby girl on June 29, 1990, but within minutes, his tiny patient was in respiratory distress. In fact, Luecke had moved to his next case — a surgical telemedicine consult — when he learned about Aida’s condition. Luecke asked the surgeon online if there was a neonatologist available in Lubbock for an emergency consult — putting TTUHSC’s fledgling telemedicine program to the test.

Read More
- No Service Interruptions
- “During the pandemic, many of my staff members have been in and out of quarantine or sick with COVID-19. Thanks to telemedicine technology, I don’t have to cancel or reschedule appointments with my patients. It’s business as usual, just on Zoom rather than in person.”
- Convenient
- “I have a webcam that I can hook up to my computer, but I find it’s easier to use my phone, which is how I conduct all of my video calls. I can handle the scheduled appointment from anywhere at any time, which only better serves my patients during the public health emergency and forever after.”
- Easier for Rural Patients
- “Our clinic’s service area is large — we extend out to Colorado, Kansas and New Mexico as well as most of Texas — and this has helped us remain a resource for patients who travel hundreds of miles to receive service. While I believe the initial patient intake should be in person, that wasn’t always possible during the pandemic. The most important thing about telemedicine to me is that it makes health care accessible during times of crisis or where health care is scarce.”
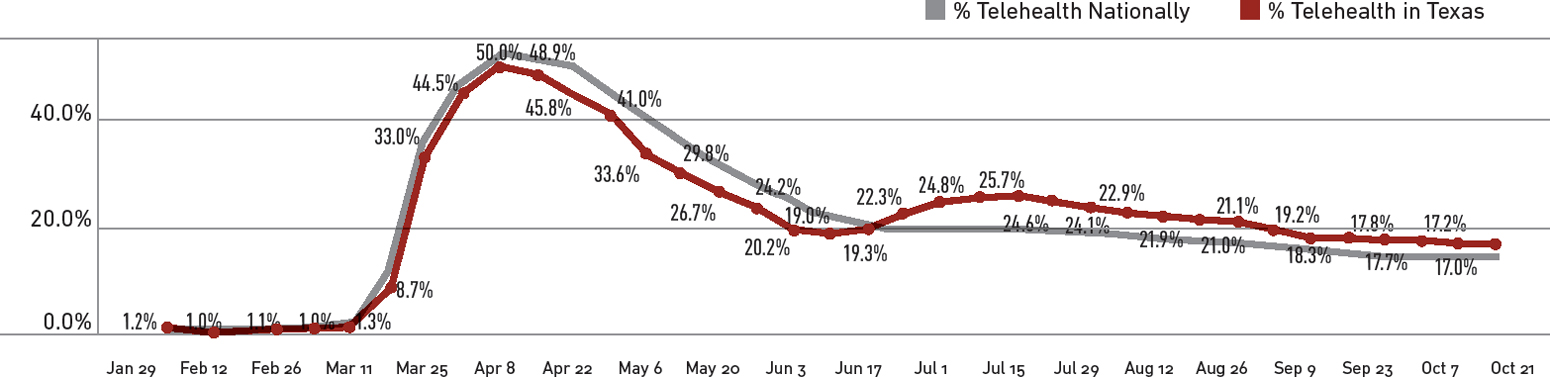
Before the pandemic, telehealth and telemedicine made significant strides toward prominence as health care delivery models and gained popularity among many medical specialists. However, there were key barriers to adopting telehealth and telemedicine as primary care mediums. Medicaid and private insurance companies were resistant to reimbursing physicians for telemedicine visits and denying reimbursement to all other providers. Likewise, there was provider resistance as it would require an investment in telehealth training, while also potentially less efficient up front due to the learning curve.
Rather than being driven by consumer demand, political will or investment potential, telehealth and telemedicine were driven by the most important factor of all: necessity.
When the pandemic entered the U.S. and shelter-in-place ordinances were established, providers and hospitals needed telemedicine onboarding — and they needed it yesterday. In less than a week, the School of Health Professions Department of Speech, Hearing and Language Sciences flipped their entire clinical practice into a remote environment. TTUHSC’s Information Technology division worked around the clock beefing up bandwidth for the transition, while TTUHSC providers and patients alike became more acquainted with video conferencing software.
“The need for services has amplified during the pandemic, and I’m glad that the third- and fourth-year residents I supervise had some familiarity with the process before the public health emergency,” said Terry McMahon, MD, professor, in the School of Medicine Department of Psychiatry, which began telemedicine in September 2019 on a trial basis in its residency program. “I was interested in telemedicine in educational training, but I also wanted to see if this was a modality we could use to extend psychiatric services.”
- The U.S. Department of Health and Human Services Office of Civil Rights implemented unprecedented waivers to the enforcement of HIPPA (privacy laws) with regard to both telehealth platforms and business associate agreements.
- Centers for Medicare and Medicaid Services (CMS) allowed the patient’s home to serve as an eligible originating site for the purpose of reimbursements.
- The CMS waived the requirement that a doctor of medicine or osteopathy be physically present to provide medical direction, consultation and supervision of services for critical access hospitals, allowing physicians to supervise remotely.
- The U.S. Department of Health and Human Services Office of Civil Rights implemented unprecedented waivers to the enforcement of HIPPA (privacy laws) with regard to both telehealth platforms and business associate agreements.
- Centers for Medicare and Medicaid Services (CMS) allowed the patient’s home to serve as an eligible originating site for the purpose of reimbursements.
- The CMS waived the requirement that a doctor of medicine or osteopathy be physically present to provide medical direction, consultation and supervision of services for critical access hospitals, allowing physicians to supervise remotely.
The importance of the patient, provider and practitioner experience throughout this pandemic cannot be understated. In our minds, medical care has always been conducted in a brick and mortar clinic, physicians in white coats wearing analog stethoscopes, and a lollipop or stickers for children at the end of the appointment.

Read More
It can be challenging to provide mental health services for students because they’re only here temporarily.
“They go home for holidays and in between semesters, making it difficult to follow up with their medication regimens or address difficulties they’re going through,” Spiegelberg said. “Then once they graduate, they lose health care services including mental health, which creates a gap in services until they are able to establish care through their employer.”
The Student Wellness Center implemented telemedicine for the COVID-19 pandemic for patient visits, which also allows Spiegelberg to fill in the gaps of mental health care beyond what she could do before.
“As long as patients stay in Texas after graduation, I am able to move them to my adult psychiatry clinic to prevent gaps in mental health services. The opportunities are endless with telemedicine capabilities in this area,” she added. “They have to extend the waivers that are allowing us to use these services — it’s making a difference for my patients, which is good for my mental health as well.”
Student exposure to and experiences with telehealth also increased dramatically with the pandemic. While younger generations are well-versed in digital mechanics, there are some unique challenges to virtual health care you wouldn’t necessarily think about — like making eye contact with a patient when using a separate web cam.
“It’s difficult to express empathy for your patients when you’re looking through a computer screen,” said Ariel Santos, MD, MPH, associate professor, School of Medicine Department of Surgery and director of the Texas Tech Telemedicine Program. “Bedside manner is very important regardless of where the bed is.”
Speech-language pathologists are also innovatively addressing challenges presented by a virtual visit. “The games we would play in person to keep our young patients engaged to improve their speech needed to be implemented into our virtual visits,” said Brittany Hall, MS, CCC-SLP, (Health Professions ’05, ’03) assistant professor in the School of Health Professions Department of Speech, Language and Hearing Sciences. “This requires additional Zoom skills that we teach our students such as building games with software and operating them through the Zoom platform.”

Read More
“We had also scheduled an appointment with (TTUHSC) when we were originally calling around, so we decided to keep that appointment. They didn’t make us start over. We had the second surgery and were immediately referred to Brittany.”
Brittany Hall, SLP-CC, MS, (Health Professions ’05, ’03) is an assistant professor in the School of Health Professions Department of Speech, Language and Hearing Sciences. For five years, she saw Antonio in person, requiring travel for the Paezes. However, the past two years have been via telepractice, which has dramatically improved the Paezes quality of life.
“The traveling was a struggle for us,” Laura said. “We have four other children, so before the telepractice, my husband would have to take off work to either take Antonio or watch the girls so I could go to the in-person appointments. Now that we’ve been using telepractice, Antonio enjoys speech so much more. It doesn’t take him out of school, and he doesn’t have to spend hours in the car.”
Antonio is now 12 years old and telepractice enables him to engage with applications, presentations and conference calls while doing therapy, making therapy more appealing through technology.
The Paezes’ youngest child, Joaquin, has cochlear implants as well. Generally, during an in-person speech session, the parent waits in the lobby while the child is in therapy. Telepractice involves the parent/guardian directly into the therapy session.
“I am an active participant in Joaquin’s sessions now, which allows me to learn and help continue his therapy techniques throughout the week in everyday activities and situations, rather than just once a week with a therapist,” Laura added. “There are so many advantages to telepractice — anyone can partake in this opportunity and reap multiple benefits.”
“Wouldn’t it be great if the primary care doctor could visit with the patient and, based on their needs, patch in the specialist to the visit, rather than referring the patient and setting up an additional appointment? We aren’t quite there yet, but I now see it as an upcoming reality.”
The Texas Tech Telemedicine Program is currently working on infrastructure to connect pharmacy, laboratory and imaging (like X-ray) to virtual primary care visits.
TTUHSC’s Correctional Managed Health Care Program’s use of telemedicine for vision care is one example. The state mandates vision screening for all offenders as they come into a correctional facility. Before telemedicine, TTUHSC had to find an optomestrist to visit all 23 facilities at 18 different sites, or transport the offenders to a location for screening. Now, with tele-optometry equipment at every correctional facility, a technician makes rounds utilizing the equipment and sends screening data to optometrists and ophthalmologists to review. Only the offenders needing additional vision care are sent offsite for further evaluation.

Read More
The TTUHSC Managed Care Program is the first correctional care program in Texas to become accredited by URAC — the nation’s largest and most experience telehealth accreditor — in 2020.
“Telemedicine is cost-efficient, enhances access to care, promotes public safety and provides better utilization of our providers. Conserving state resources makes telemedicine very attractive to correctional health care.”
The program is under a statuary mandate to provide vision screening for all offenders as they come into a correctional facility. Before telemedicine, Jumper said, they had to find an optometrist to visit all 23 facilities at 18 different geographical sites or bring the offenders into the John Montford Unit in Lubbock for screenings.
Now, with tele-optometry equipment at most facilities, a technician makes rounds, utilizes the equipment and sends the screening data to optometrists and ophthalmologists to review. Only the offenders needing additional vision care are sent offsite for further evaluation.
In the spirit of conserving resources, managed care also has switched to centralized scheduling.
“If the facility in Dalhart, for example, goes into lockdown and the offenders cannot be virtually seen, the provider in Dalhart can be rerouted to help another facility catch up on its patient load,” Jumper added. “Also, when a doctor is going to be gone for two weeks, I can put another provider on his or her virtual caseload without having to hire an additional provider to cover the two weeks.”
“We’ve always used telemedicine in some form,” Jumper said. “Now, we have the opportunity to further improve on an already efficient system.”
- Express empathy and compassion through tone of voice.
- Listen and be patient — bandwidth can cause delays or break connections. Take notes while patient is talking to prepare a response.
- When using a separate webcam, position it in the middle of your computer screen so you are making eye contact with the patient.
- Perform the virtual visit in a quiet space and avoid distractions by muting your phone, etc.
We are all currently participants in a great experiment — implementing and waiving policies and procedures to meet the needs of public health, the consequences of which will only be fully appreciated after the fact.

Read More
Q: What has been the patient response to using telemedicine during the pandemic?
A: Since the enactment of waivers expanding access to telemedicine services, our clinics have embraced the opportunity to serve our patients both virtually and in person. Depending on patient preference and/or medical case, telemedicine may be a potential health care access point, so response has been varied. It is important to remember that barriers to care do not look the same for everyone in our communities. While telemedicine services are convenient for some, they remain cumbersome and elusive for others.
Q: Do you believe that patients will come back for in-person clinic visits, or will they more often prefer the virtual option?
A: There are great reasons why, depending on the health question or need, either in-person visits, virtual visits or a mix of both could be the best option for patients moving forward. Therefore, I hope that the advent of greater telemedicine use leads to both greater access to care and partnership between patients and their health care teams. Telemedicine can be a powerful way to overcome time and travel barriers to care, but there are times when the qualities of in-person communication and physical examination will be paramount.
Q: Are there any negative ramifications to health care infrastructure if telemedicine’s current prominent role became permanent?
A: Without further improvement of the telemedicine experience, we could actually disenfranchise members of our communities who benefit the most. More must be done to address challenges that affect our most vulnerable patients, namely the elderly and socioeconomically disadvantaged. Many of our elders are not digital natives; therefore, we should be open to their preferences and feedback to make health care work well for them. Additionally, much of the current usage of telemedicine is in the areas of acute care visits. Still, we must not lose sight of continuing to provide important preventive measures like vaccines, screenings and regular physicals for all.
Q: How long have you used telemedicine?
A: My first exposure with telemedicine was during residency training, but it was limited to seeing its application in a few special circumstances to connect patients with specialists not available in our area. My experience with telemedicine started in earnest with this pandemic. Beforehand, logistical and regulatory barriers such as requirements for specific software and equipment made the use of telemedicine difficult for many patients and physicians.
Q: Would you like to see the waivers granted during the pandemic permanently upheld after the emergency declarations are no longer in effect?
A: Yes. Extending the telemedicine waivers granted during this pandemic will allow health care teams to continue to innovate on the delivery of convenient and comprehensive care.
When the dust settles after COVID-19 and we finally look back to evaluate how the pandemic has affected health care delivery, operating costs, incomes and patient outcomes, the resulting data will undoubtedly be used to advocate for reforms that encourage greater implementation of telemedicine and telehealth, including permanent implementation of many of the temporary waivers currently in place.
Whether it’s saving the life of a newborn or examining a sprained wrist during a pandemic, TTUHSC’s objective in using telemedicine and telehealth remains the same now as it did 30 years ago: provide the best level of care and ensure the best quality of life for every patient no matter what comes over the horizon.