By Kara Bishop
By Danette Baker

Yet, it’s in the messy middle that new ideas are born; new collaborations occur. The stories in this issue are a testament to that. In the middle of this mess, we know as the COVID-19 pandemic, the future of health care and TTUHSC is taking shape.
Our faculty and staff have delivered exceptional health care education online for many years. COVID-19 brought an opportunity for innovation in delivering virtual experiences in simulation and gross anatomy as well as other areas.
We volunteered at home and in New York. We invented new ways to produce testing supplies and much needed personal protective equipment and shared that knowledge with others. We made N95 masks reusable. We fed front-line team members, found places for them to stay, and we gave generously to support these efforts.
That’s what this issue is about — the incredible connection and service of the TTUHSC family responding to the coronavirus pandemic. We know there are countless stories of heroism that we didn’t include and may not have known about, so we tried to capture the spirit demonstrated in these uncertain times.
This issue, we are launching a new digital platform for Pulse — the second phase of our redesign. Our goal is to provide a richer experience and easier read of our online content.
This format allows you to easily access and share Pulse on mobile devices — whether you are reading it on a desktop computer or smartphone. There’s no flipping or getting lost in our new digital platform, simply scroll down. We hope you enjoy this format and will be releasing the option to receive the digital issue only, if you prefer it to print. When you fill out the follow-up survey, simply state your preference.
We chose to print a digital-only version of this issue, so we could contribute to TTUHSC’s COVID-19 relief efforts. The Winter 2021 issue will be published in both print and digital formats.
If you have a story request or would like to provide feedback on this issue, contact us at pulse@ttuhsc.edu.
We hope you are well and stay safe.
Office of External Relations

Through survey responses, we have learned a great deal about our magazine and how to produce the best product for the readership. If you wish to be involved in the process of what goes in your magazine, please make sure to respond to the survey.
As always, if you have a story idea, please submit it to pulse@ttuhsc.edu.
Danette Baker, MA
Kara Bishop
Jim Nissen
Suzanna Cisneros, Meaghan Collier, Stephanie DeFranco, Kate Gollahon, Mark Hendricks, Neal Hinkle, Emily Holeva, Heather Houser, Kami Hunt, Jo Grant Langston, Tessa Meriwether, Tiemdow Phumiruk, MD, (Medicine ‘97) Caroline Wahl, Melissa Whitfield, Glenys Young, Ben Zweig
Lori Rice-Spearman, PhD
(Health Professions ‘86)
Ashley Hamm
Mattie Been, Amarillo
Jessica Zuniga, Permian Basin
Cyndy Morris
Smiley Garcia, Clifford Wilkes
pulse@ttuhsc.edu
TTUHSC External Relations
3601 Fourth Street 6242 6238
Lubbock, TX 79430-6238


Second Degree Bachelor of
Science in Speech, Language,
and Hearing Sciences
Master of Science in Speech-
Language Pathology
Doctor of Audiology
Second Degree Bachelor of Science in Clinical Laboratory Science
Post-Baccalaureate Certificate in Clinical Laboratory Science
Master of Science in
Molecular Pathology
Master of Physician
Assistant Studies
& Mental Health
in Addiction Counseling
Master of Science in Clinical Mental Health Counseling
Master of Science in Clinical Rehabilitation Counseling
Graduate Certificate
in Veteran Services
Doctor of Occupational Therapy
Post-Professional Doctor of Occupational Therapy
Doctor of Physical Therapy
Doctor of Science in
Physical Therapy
Doctor of Philosophy in
Rehabilitation Science
Doctor of Occupational Therapy
Post-Professional Doctor of Occupational Therapy
Doctor of Physical Therapy
Doctor of Science in
Physical Therapy
Doctor of Philosophy in
Rehabilitation Science
Healthcare Management & Leadership
Bachelor of Science
in Healthcare Management
Master of Science
in Healthcare Administration
Graduate Certificate
in Health Informatics
and Data Analysis
Graduate Certificate
in Health Systems Policy
and Management
Graduate Certificate
in Healthcare Finance
and Economics
Graduate Certificate
in Health Systems
Engineering
and Management
Graduate Certificate
in Long Term Care
Administration
As the outbreak progressed, TTUHSC followed public health recommendations and CDC guidelines for the safety of TTUHSC faculty, staff and students.
For the next three months, the majority of the TTUHSC workforce and students stayed off campus. Zoom meetings and other virtual communication became our new normal. Nevertheless, we followed the instruction of leadership and kept increasing momentum. As Rice-Spearman has daily reminded us: this is TTUHSC, and we’re all in this together.
 All together ttuhsc
All together ttuhsc
- Step 1:
- Remove all personal protective equipment in exam room — gown, scrub cap, goggles, mask, gloves — following standard procedure.
- Step 2:
- Arrive home and remove all clothing in the garage. Head straight to washing machine and deposit discarded clothing — start cycle.
- Step 3:
- Immediately shower, disinfect all doorknobs and everything else that was touched on the way to the bathroom.
- Step 4:
- Clean bathroom.
This is how Jessica Gray, MD, (Resident ’18, Medicine ’15) ends a work day. Volunteering to work the COVID-19 Drive-Through Screening at UMC Health System, and maintaining her family medicine practice with UMC Physicians, demands it.
Gray always knew she wanted to be a doctor — even graduating high school early to get a head start. She also knew she would attend Texas Tech University for her undergraduate degree and medical school at TTUHSC. She just knew. “And, for the first time, I’m nervous about going to work. I’m a little uncertain, yet still so proud to serve as a physician amid COVID-19.”
Missed It…
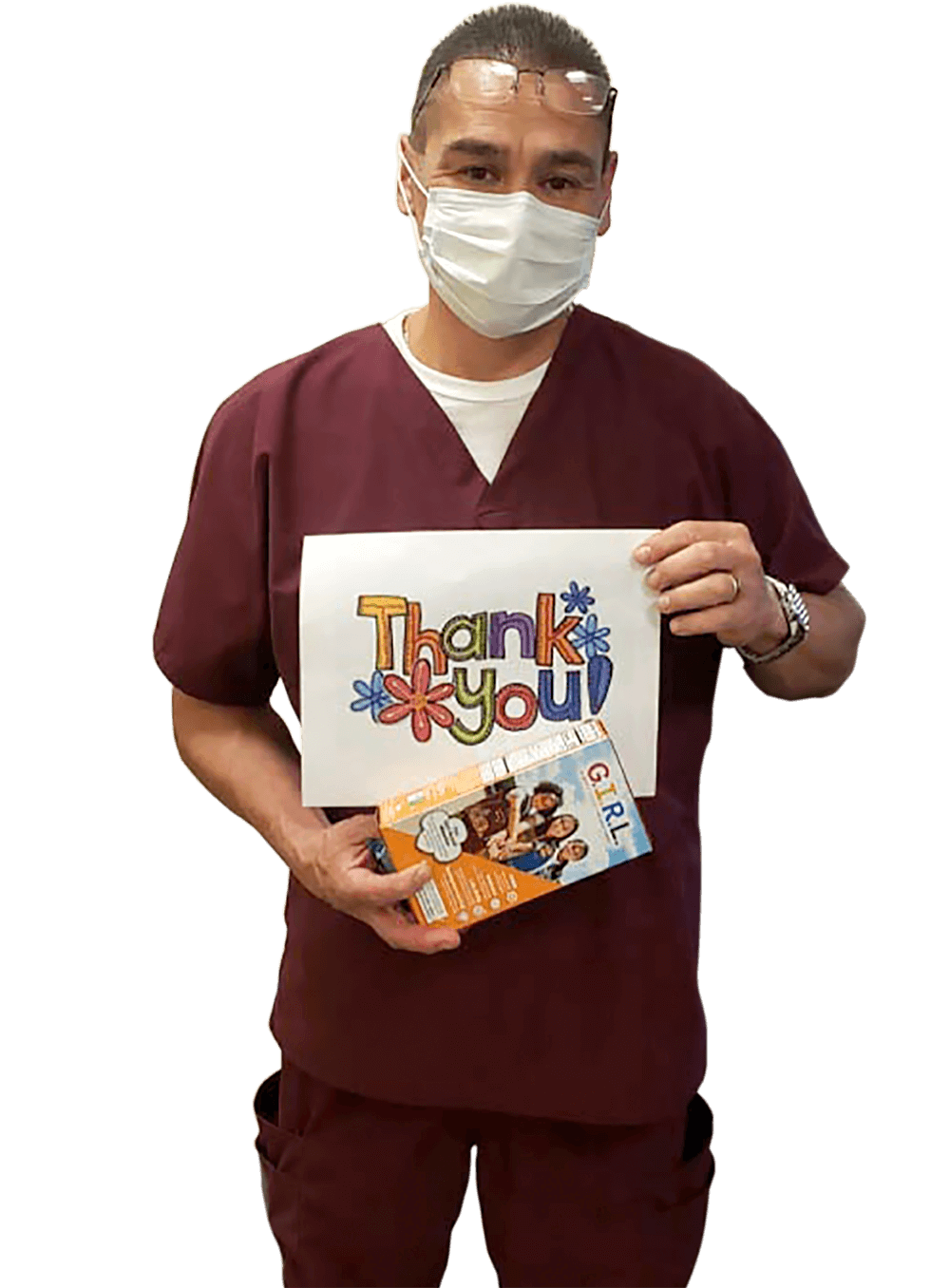
The initial goal of $4,000 was easily exceeded, and TTUHSC LMSA was able to purchase gift cards for each custodian.
“The custodial staff is an essential part of the front-line health care team,” Ochoa said. “They’re the ones who clean up fluids after surgery and examinations. We can’t do our jobs as doctors and nurses if we don’t have a sterile environment to work in.”
“TTUHSC’s access to partnerships in our communities allows us to deliver the latest treatment options to patients in West Texas,” said TTUHSC Executive Vice President and School of Medicine Dean Steven Berk, MD. “We were able to shepherd this project into the area within 48 hours.”
Plasma collected from recovered COVID-19 patients is infused into infected patients. Sick patients may benefit from antibodies produced by the recovered patients.
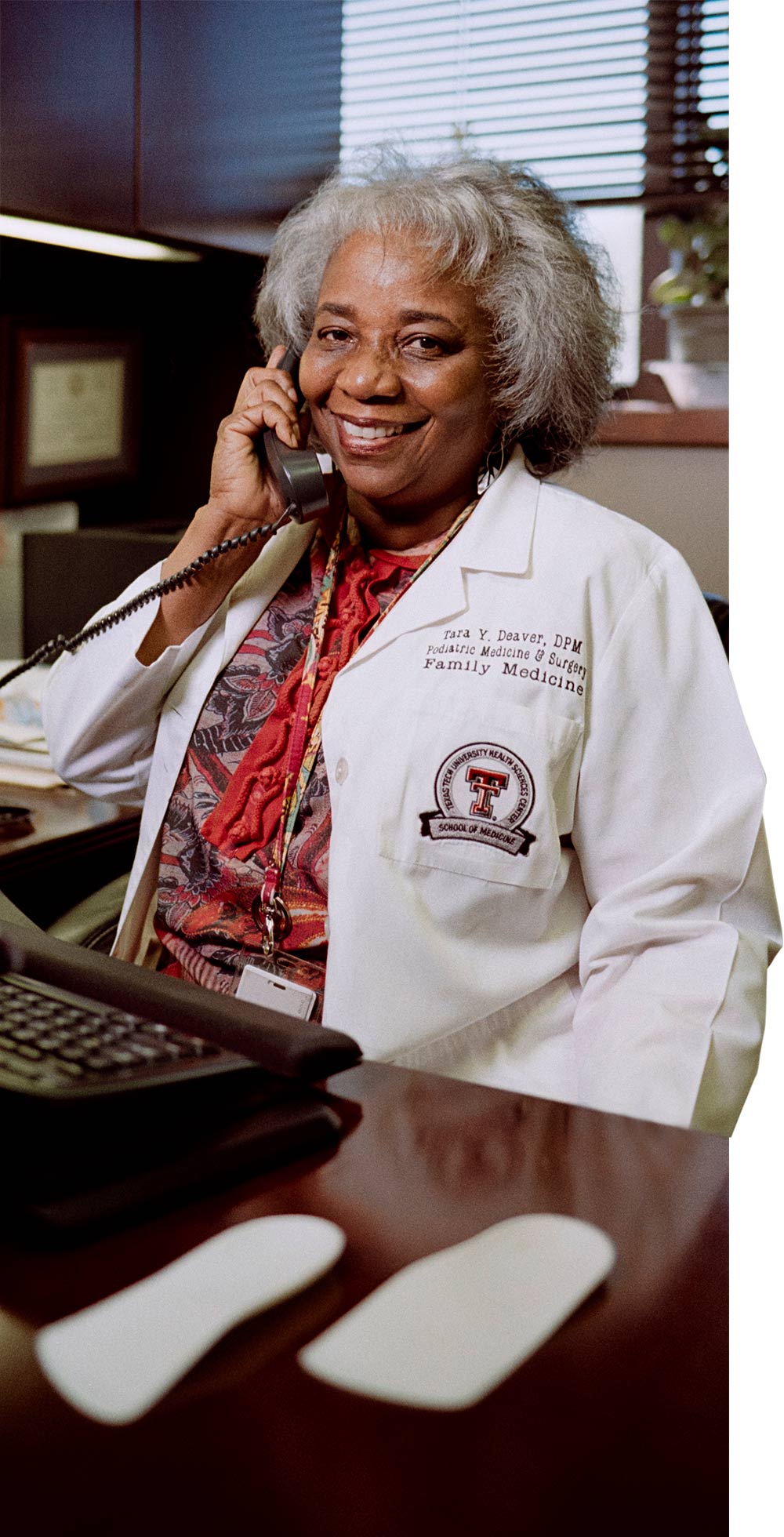
 FACULTY PROFILE
FACULTY PROFILE

Permian Basin
 for the record
for the record
FREE

When COVID-19 spread through the U.S., health care supply shortages spread with it. To provide proper personal protective equipment for front-line health care workers, the West Texas 3D COVID-19 Relief Consortium was formed. The consortium, a collaboration of entitites within the Texas Tech University System and community partners, began an initiative to create 3D-printed face masks and face shields. And the great thing about 3D printers? You can use them anywhere.
 School of Medicine
School of Medicine
Q: Why is this residency important?
A: This residency is unique in the way it teaches doctors to approach patients. We call it “the first 15 minutes” in emergency medicine, because you need to know a little bit about everything rather than focusing on one system. Instead of looking for most likely scenarios when patients exhibit symptoms, emergency medicine physicians are looking for what is going to kill the patient or symptoms with the highest priority.
I was born and raised in West Texas, went to medical school at TTUHSC, but was forced to leave for my residency. We are excited for the opportunity to now offer an emergency medicine specialty, so our students don’t have to leave West Texas to train.
Q: How accurate are the trauma situations in TV medical dramas such as “Grey’s Anatomy?”
A: The medical scenarios are pretty accurate; however, it’s the multiple rare cases that you normally might see once every 10 years all happening in one hour that’s not accurate. They leave out the bread and butter of emergency medicine, which is regular abdominal pain, shortness of breath, chest pain, etc.
Q: Will the residency be delayed or affected by COVID-19 in any way?
A: No. We have ensured that each resident is properly equipped with protection against COVID-19, but you go to medical school to take care of sick people. So that’s what we all will do.
 School of Medicine
School of MedicineMid-March, the beginning of the COVID-19 outbreak in the U.S., the Brownfield Regional Medical Center had a possible COVID-19 case — and a need for more N95 masks as medical professionals are trained to dispose N95s after one use.
Michael Tackitt, LP, CRHCP, director of the medical center’s rural health clinic and emergency medicine manager, watched his healthy supply of N95s dwindle as days went by. Tackitt read a news article about Team Decon — an effort led by Min Kang, PharmD, TTUHSC’s interim senior vice president of research — decontaminating N95 masks.
Kang and her team of medical and biomedical sciences students researched decontamination methods using hydrogen peroxide vapor. They then sterilized the masks by fumigation in a large chamber. When evidence revealed the process to be efficient, Team Decon opened the service to hospitals and clinics.
 School of Health Professions
School of Health ProfessionsAfter months of exhaustion, failing to interact with peers, and craving a nap instead of participating in after-school activities, sixth grader Angelica Rodriguez was diagnosed with hearing loss. The year before she had sustained minor injuries from a car accident, but there was no indication she would suffer long-term consequences.
The diagnosis told her what was wrong, which helped, but that’s all it told her. Rodriguez began to dread the doctor appointments where they would tell her, yet again, how her hearing loss was equivalent to that of a construction yard worker who had been around heavy machinery for 20 years. Doctors and specialists continually told her what she couldn’t do and what her limits were.
It wasn’t until she was a junior in high school that she met an audiologist with a different point of view — she wasn’t broken and hearing amplification devices didn’t make her weak. After refusing to use amplification for years, she began to enjoy life again with the help she needed.

 School of Health Professions
School of Health Professions
Adjunct Faculty and Regional Coordinator, Master of Science in Physician Assistant Studies
medical and health service managers
 Jerry H. Hodge School of Pharmacy
Jerry H. Hodge School of PharmacyWhen Gov. Greg Abbott published “The Governor’s Report to Open Texas” in April, he commended TTUHSC for producing viral transport medium (VTM) to expand COVID-19 testing access.
VTM is a sterile tube with 1mL to 3mL of cell culture media that contains a broad-spectrum antibiotic and an antifungal agent. The VTM protects the virus samples obtained from nose or throat swabs. Since the coronavirus is particuarly unstable, it’s important the samples don’t degrade in transit to processing facilities. Any changes could lead to incorrect testing results.
“While we didn’t have VTM in our labs, a literature search revealed that it could be prepared in-house from materials that are readily available in many labs doing cell culture work,” said Ulrich Bickel, MD, professor and associate dean of the Department of Pharmaceutical Sciences in Amarillo.

 JERRY H. HODGE SCHOOL OF PHARMACY
JERRY H. HODGE SCHOOL OF PHARMACY
 JERRY H. HODGE SCHOOL OF PHARMACY
JERRY H. HODGE SCHOOL OF PHARMACY
Staci Moss, PharmD, (Pharmacy ’02) assistant professor in the Department of Pharmacy Practice, has always found a way to achieve her goals while living with chondrodysplasia punctata syndrome. Patient education was one of her favorite aspects of the job — until the COVID-19 outbreak changed everything.
“This is the first time I’ve actually not been able to do what I wanted to do,” she said. “I’ve always found a way around my obstacles before, but now, because I’m a high-risk employee, I’m not allowed in the pharmacy.”
While at home during the emergency remote work operations instated by TTUHSC, she assumed she would have to take off work. However, Moss’ determined demeanor is well known in the school, and she soon received a phone call from Eric MacLaughlin, PharmD, chair of the Department of Pharmacy Practice. “You are still a pharmacist,” he said. “And, right now, we need you.”
Since March, Moss has been facilitating student education via Zoom and working to access additional revenue streams for TTUHSC’s community pharmacies. She’s passionate about ensuring the survival of the independent pharmacy model and is working on next steps to offer compounding pharmacy services at TTUHSC.
This outbreak has affected everyone, and Moss is grateful to be in the TTUHSC family during these uncertain times.
“Even when things are difficult, everyone still has a place and purpose, and I’m thankful for that.”
Chephra McKee, PharmD, BCPPS, assistant professor in the Department of Pharmacy Pracitice, Pediatrics Division in Abilene, provides insight on vaccinating children during a global pandemic.
Q: Why do you think it is important to continue to vaccinate children amid a global pandemic?
A: COVID-19 should not deter us from taking a proactive approach toward the diseases we do have vaccinations for. We should use the resources we do have to protect our children no matter what circumstances we’re facing.
Q: Why is it necessary to stay on target with vaccination schedules?
A: Vaccines are scheduled at times that are most appropriate to help protect children against preventable diseases. The schedules that are published each year have been shown to be the most effective at creating an antibody response in children to protect them from these diseases.
Of course, we know that life happens and occasionally people may get behind on vaccines. Parents can discuss this with their child’s pediatrician to help get back on track. -Caroline Wahl
 Graduate School of Biomedical sciences
Graduate School of Biomedical sciencesRotors stall and the helicopter carrying Ryan Baxter does a 180-degree dive into the water. Disoriented with limited vision in the murky water, Baxter, MD, MS, (Medicine ’17, Biomedical Sciences ’13) has minutes to unstrap his safety harness and fight his way to the pool’s surface. He successfully emerges. Today’s drill is over.
As an aerospace medicine resident with the U.S. Navy, Baxter undergoes intense training drills in the “helo dunker” to prepare him for military service.
“A helicopter’s machinery is at the top, so every time you crash in water, you’re going to almost immediately flip upside down,” Baxter said. The helo dunker simulator trains soldiers to adapt to the disorientation. Pilots are strapped in the simulator and “dunked” into a pool. The device flips them upside down, imitating a helicopter crash in water. They then must escape the chopper and swim to safety.
This is just one of the many egress tests that Baxter must complete during residency. Inspired by his uncles, both who were in the U.S. Air Force, Baxter has always known he wanted a career where he served his country and his fellow man.

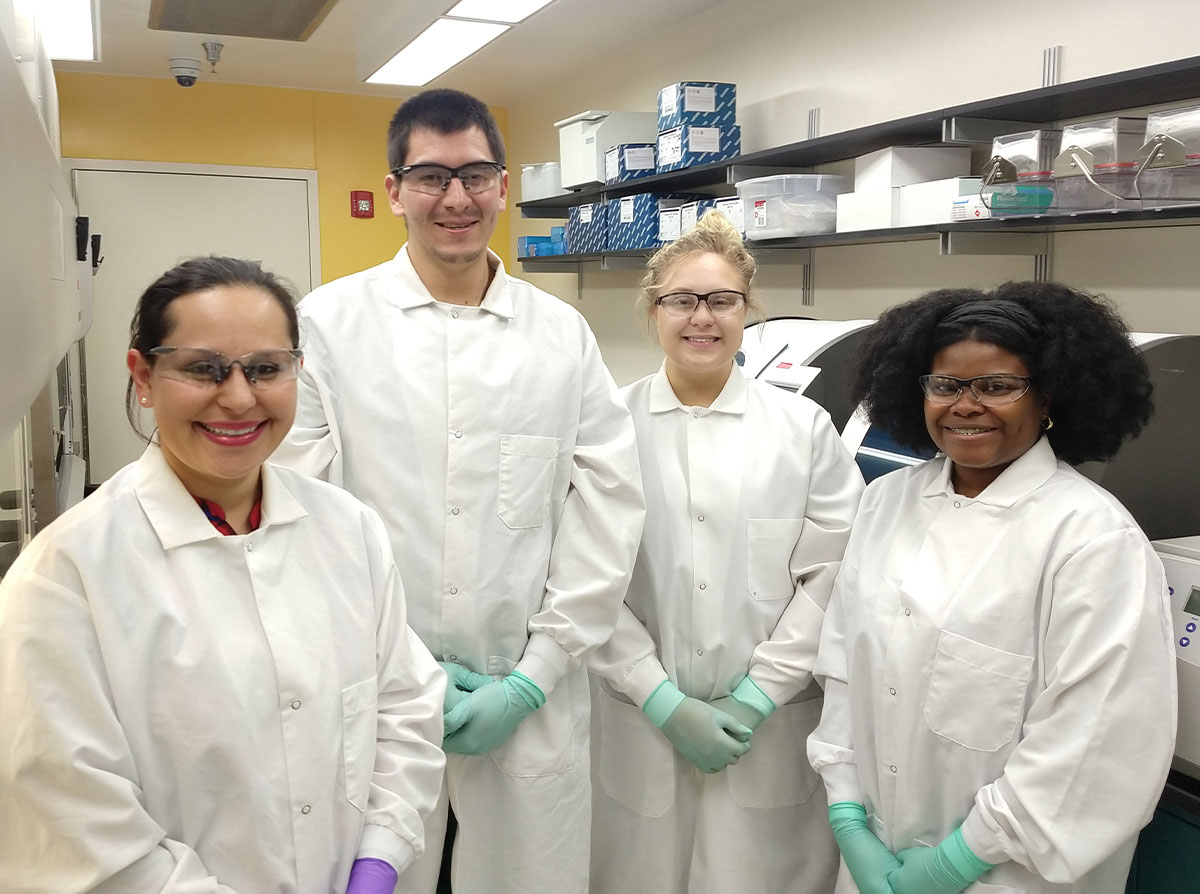
As COVID-19 continues to make history, TTUHSC students have stepped up to do their part. Cynthia Reinoso Webb, PhD, (Biomedical Sciences ’17) is the biological threat coordinator and general manager of the Texas Tech University Bioterrorism Response Laboratory (TTU BRL) at the Institute of Environmental and Human Health. She received inquiries about volunteering from over 50 TTUHSC students within the first few days of establishing a COVID-19 test processing site as part of the Centers for Disease Control and Prevention (CDC) Laboratory Response Network. The TTU BRL was the first in the state to process COVID-19 tests.
Josue Enriquez was one of those 50 students. “It just seemed like the right thing to do,” said Enriquez, a PhD student in the Department of Immunology and Molecular Microbiology. He was one of the first students to volunteer to help in the TTU BRL. He works for seven to nine hours screening test samples until the next round of volunteers come in. The lab processes samples seven days a week.
The TTU BRL serves Lubbock County and 66 others in the region as a reference laboratory for biological threats and emerging diseases. COVID-19 test results are provided within 24 hours. After swab samples are submitted to the lab from hospitals and clinics, they are processed and analyzed for traces of the coronavirus using the CDC real-time RT-PCR test. The results are then interpreted by highly trained personnel and reported to federal, state, regional and local health agencies.
As of press time, the TTU/TTUHSC COVID-19 testing team can process over 350 samples each day. More than 5,000 samples have been tested so far. – Caroline Wahl
 School of Nursing
School of Nursing Neither alumna was completely prepared for the reality in the northeast, but they both made it work and honored their profession. Springfield worked tirelessly to keep her patients comfortable in spite of a drug shortage, while Enlow finally repaired the oxygen port in her patient’s room herself, so he could have access to oxygen without needing a tank.

TTUHSC came together
as the COVID-19 outbreak raged,
because we saw
Connection
wo years ago, Tobi Saliu walked into her medical school interview at TTUHSC not sure what to expect.
West Texas was unfamiliar to this Dallasite, but she was open to exploring new possibilities. Her determination to find the right place resulted in interviews at multiple medical schools. This due diligence led Saliu to Lubbock and eating breakfast with then TTUHSC President Tedd L. Mitchell, MD.
This is weird, she thought. I didn’t even approach the deans at the other medical schools, and here the president not only greeted every candidate, I’m eating breakfast with him.
This campus had a vibe she couldn’t quite place, but it felt like home.
In her first interview, Saliu listened to Mimi Zumwalt, MD, (Resident ‘96) professor in the School of Medicine Department of Orthopaedic Surgery, introduce her to a fourth-year medical student. “I didn’t have to say anything,” Saliu added. “She knew my whole story.” The interview itself was a personable conversation about hobbies and interests as much as it was academics.
Her second interview went much the same way as Saliu found herself discussing her favorite food with Shaughn Nunez, MD, (Resident ’14; Medicine ’11) assistant professor in the School of Medicine Department of Pediatrics. While Saliu’s qualifications were meticulously reviewed, she never felt the stress that had accompanied her to other medical school interviews.
She’s not the only one. Many students report a family-friendly atmosphere when they walk on campus for the first time. At all five campuses, TTUHSC connects first — it’s the principle cultivated from the very beginning of employment or academic acceptance.
That connection just grew stronger as the COVID-19 pandemic moved closer to home.

t the moment, I want to be a general surgeon,” said third-year medical student Ellen Wilson. “But beyond the specialty, I want to be mindful. Mindful in decision making for my patients and their families. I want to be the calm in their storm.”
Wilson’s wishes came closer to fruition as she spent three months working the TTUHSC/UMC Health System Nurses on Demand 24/7 COVID-19 Triage Hotline in Lubbock.
“People called in terrified, because they had a cough,” she added. “I tried to ease their worries and give them direction based on their symptoms.”
Wilson didn’t anticipate the TTUHSC medical student response when she posted a spreadsheet to her class Facebook page asking for volunteers to help front-line health care workers. More than 100 students signed up in the first two days.
The official TTUHSC COVID-19 Student Task Force checked temperatures at the temporary childcare center for UMC and TTUHSC front-line teams at Lubbock ISD’s Jane Ann Miller Elementary; worked the triage hotline and UMC COVID-19 drive-through screening; made masks and collected and distributed donated personal protective equipment; and assisted in research to decontaminate N95 masks, making them reusable. The task force involved students on Amarillo, Lubbock and Permian Basin campuses.
Health care training in 2020 will forever be defined by COVID-19. Years from now, maybe staff and equipment shortages, working overtime and the unique stress that has come with this pandemic will be forgotten. However, the resourcefulness and family connection gained will stay with TTUHSC students as they advance in their medical careers.
trained
Hours
students
were
featured
made and
delivered






Truly appreciate all the support!”
COVID-19 Topics

Answer
For this method to be effective, there must be a timely reporting of symptoms by infected people. Knowing how many people have been potentially exposed will help us determine strategies to contain the virus with resource allocation and health systems planning.
Regarding COVID-19, close contact is considered to be within 6 feet of an infected person for at least 15 minutes up to two days before the infected person starts developing symptoms, according to the Centers for Disease Control and Prevention (CDC).
professor and associate chair
Answer
Graduate students and post-graduates in biology or residents and fellows in medicine will be able to use the data analysis to gain a wider perspective of the problem, leading to advancements and economic activity in the future.

associate professor
Answer
The antibody test measures the presence of antibodies in the patient by testing blood samples. This test looks for the patient’s immune response that occurs after the coronavirus infection.
Longer See Me
’m not trying to complain or make excuses, I hate that I even have to ask, but I’m not able to make the deadline on this assignment,” Kenny Lam wrote in an email to Tammy Scott late one night in March. “I’ve just got a lot going on and am a little stressed out. I hate to do this, but I’m requesting an extension if possible.”
As Scott, PhD, RN, BC, assistant professor in the School of Nursing, reads Lam’s email, the words written aren’t necessarily alarming, but the tone seems off. She’s board-certified in psychiatric mental health and feels the need to reach out, even though it would be easier to just reply to the email and grant the extension. She requests a phone call and Lam, a student in the RN to BSN program, calls her immediately.
Scott learned he was working 50-plus hours a week in the medical intensive care unit caring for COVID-19 patients at UMC Health System in Lubbock.

ive hours by car separates the Dallas/Fort Worth Metroplex from Lubbock, Texas. In terms of significant health care settings, it’s a next-door neighbor. So, when the first case of Ebola was diagnosed in September 2014 — in Dallas — that was a little too close to home for Steph Hoelscher, DNP, RN-BC, CPHIMS, FHIMSS (Nursing ’19, ’15, ’95).
At the time, she was the chief clinical analyst for the School of Medicine Office of Clinical Transformation. Steph managed the electronic health records (EHR) system for the TTUHSC medical clinics.
That could have easily been us, Steph thought.
The case brought scrutiny from the public and the health care community. How could the hospital have admitted a man from Liberia twice within three days without diagnosing him with the deadly Ebola virus? The man died two weeks later, and subsequent contact tracing later revealed numerous exposures before the diagnosis, including two nurses in direct contact who became infected but fully recovered.
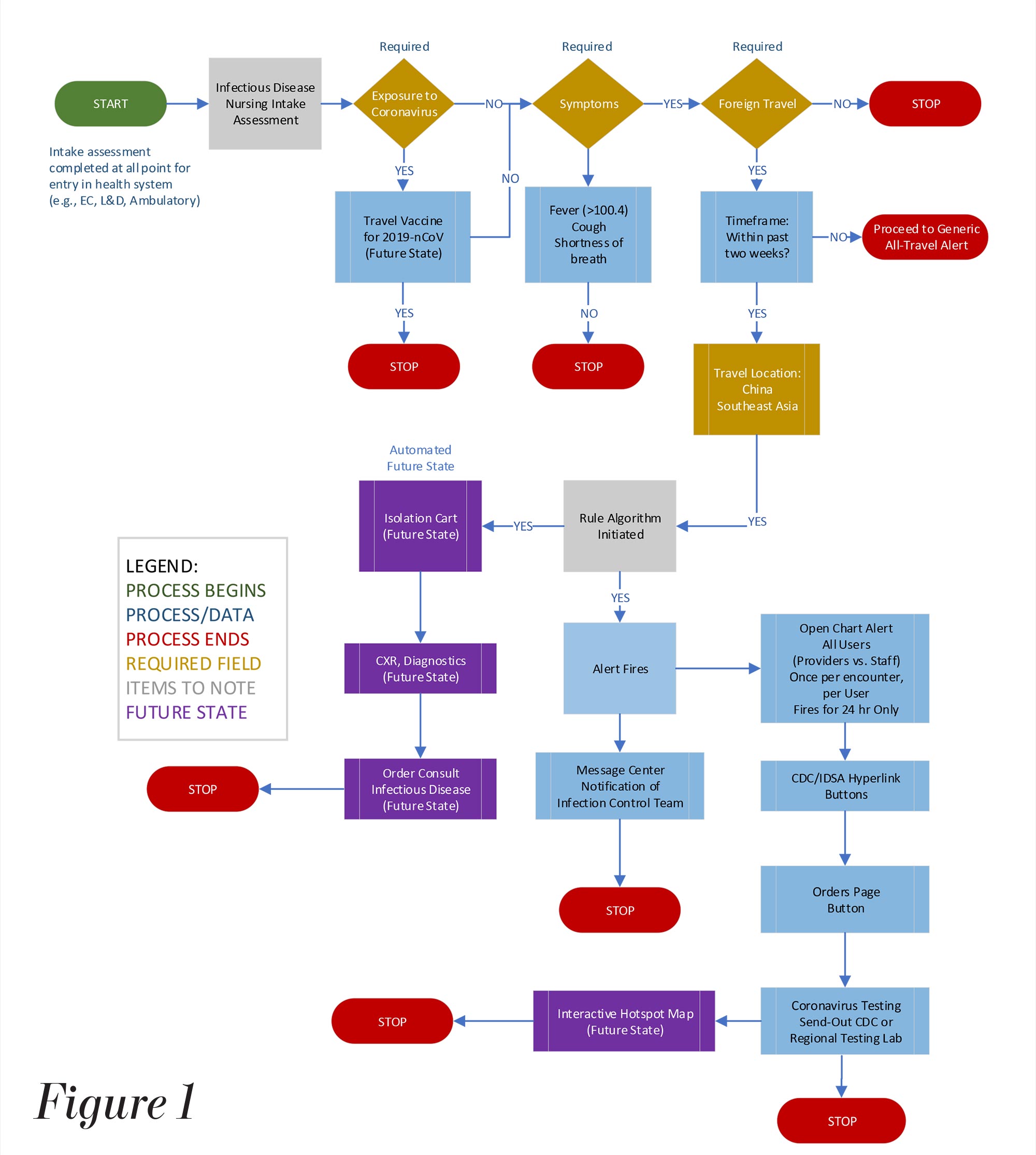
he front-line health provider opens the patient’s chart and begins with a question of known exposure to the coronavirus. From there, a yes/no decision tree guides the clinical decision process to determine the patient’s likelihood of having COVID-19.
On the surface, the workflow seems pretty straightforward; behind the scenes, an algorithm feeds from various data fields and conditional logic to support the clinical decision process. The database was developed with the input of subject matter experts nationwide.
This is the clinical decision support rapid deployment model (See Figure 1) used to diagnose and treat patients in the TTUHSC clinics and in UMC Health System’s hospital and clinics.
The Hoelschers each received grants from the American Association of Colleges of Nursing/ Centers for Disease Control and Prevention (AACN/CDC) for doctoral studies that contributed to their model. Steph’s focus was on clinical satisfaction with the model. Dwayne’s project focused on the model workflow. To read more about their work, visit the AACN/CDC website at bit.ly/2OIrHgx.
Ty Whisenant, MD, PhD, (Medicine ’19; Biomedical Sciences ’17) was a laboratory technician contracted by the state of Texas during the swine flu, or the H1N1 virus.
“I feel like we were more prepared for the coronavirus because of the H1N1 virus,” said Whisenant, now an internal medicine resident at TTUHSC. “Obviously, I’m not in the lab anymore, but the testing, at least in Texas, seems to be going more smoothly.”
Whisenant hopes that we remember the precautions for preventing the spread of COVID-19 in the future during flu season. “The flu is horrible and has killed so many. Let’s be just as cautious in terms of hygiene and going to work when the flu hits.”
 TTUHSC Steps UP
TTUHSC Steps UP
 Evolving Times
Evolving TimesMost hospitals today use an answering service to replace the pager. An emergency room doctor needs a neurosurgery consult, so he calls the answering service and leaves a message for the neurosurgeon.
It’s difficult to tell who is actually on call in each specialty as shifts change and information doesn’t always get updated. Sometimes the messages are sent to the wrong person and end up in limbo, or the person receives the message, calls back and reaches the front desk or the charge nurse instead of the doctor that actually called.
By this time, minutes the patient didn’t have in the emergency room have passed, and the consult still hasn’t happened.
Brady Anderson, MD, (Medicine ’03) a trauma and general surgeon for multiple hospitals in Austin, Texas, was fed up with this system and is bringing the pager back, so-to-speak, in a new smartphone app called PageMD.
If a hospital has their staff download the app, all doctors and nurses are listed in the directory, showing the staff who is on call and available. They can “page” the direct person they need through the HIPPA-compliant app, eradicating the inefficient answering service and health care worker burnout. In a COVID-19 world, saving minutes and frustration is key.
To learn more about PageMD, visit: www.pagemdnow.com. The app is available for download for iPhone and Android.

CITY OF LUBBOCK HEALTH AUTHORITY
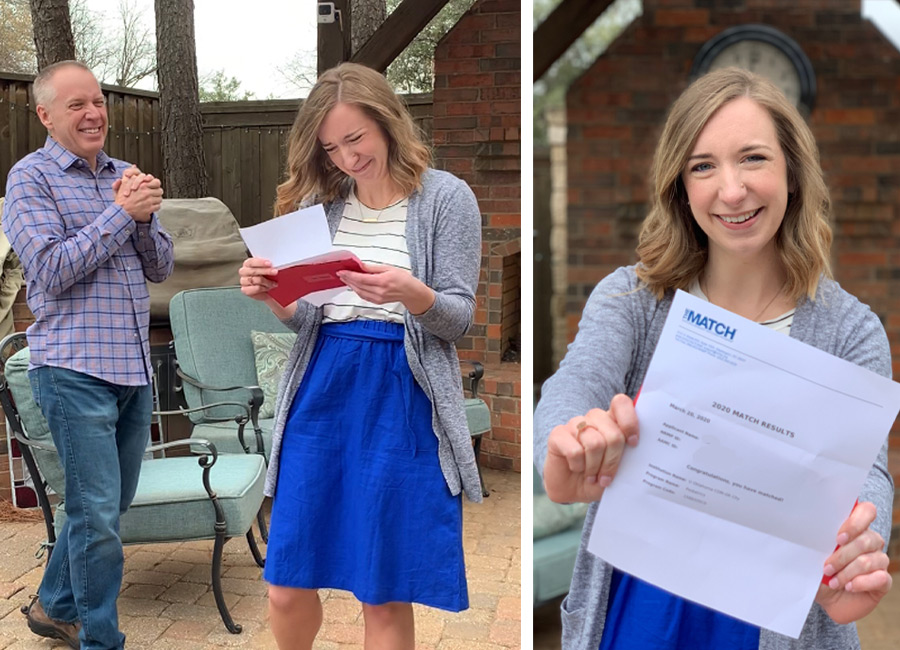
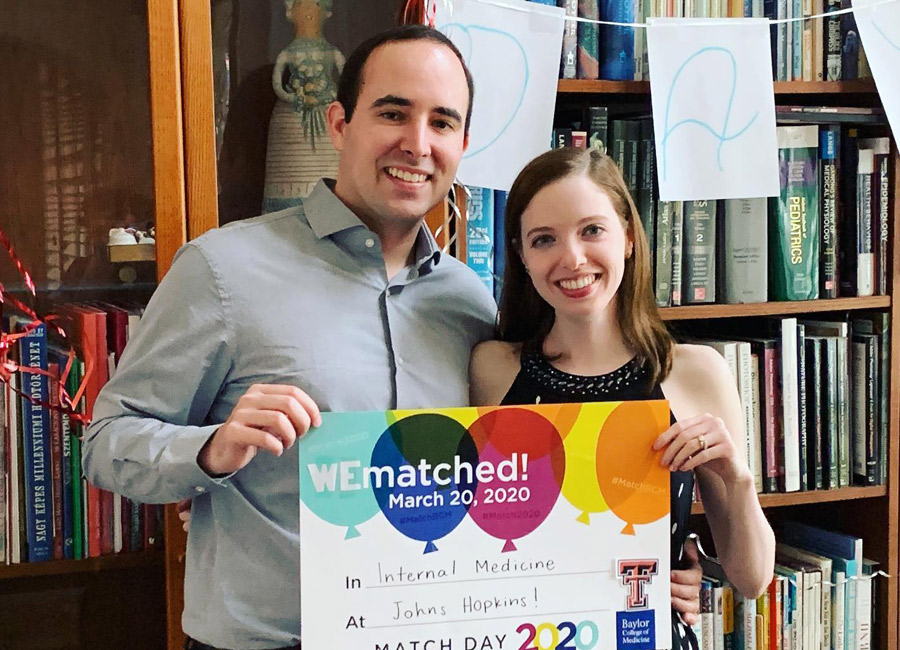
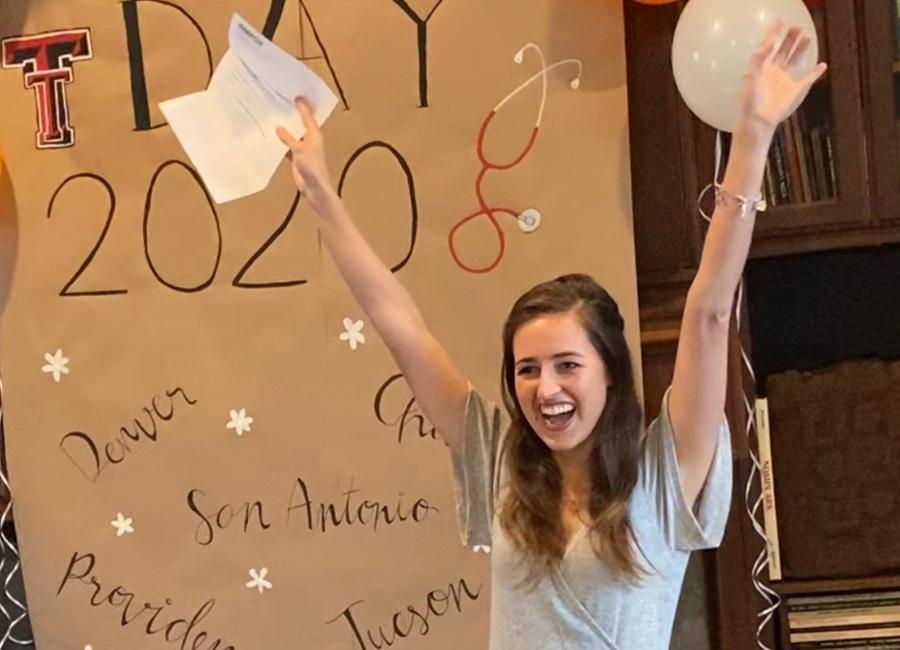
 VIRTUAL MATCH DAY
VIRTUAL MATCH DAY






1 | Stream the Match Day virtual ceremony to the TV.
2 | Gwin toasts with his wife, Josie, and daughter, Ruth, as he discovers he’s matched in pediatrics to his first choice: Children’s Mercy Hospital in Kansas City, Missouri.
3, 4, 5 | Eat all the cake, call all the family and take all the pictures! Congratulations to all of TTUHSC ‘s medical students for matching in 2020.

U.S. Food and Drug Administration,
Silver Springs, Maryland
Biomedical Sciences Graduate: 2005, 2000
Although McMahon died in 2018, Karunasena’s passion for cancer research continues.
While she loved where she worked, Karunasena needed a career change, finding it difficult to work with reminders of her late husband and their shared dreams. “In his absence, I was living in shadows, and I knew I wouldn’t be able to do that every day.”
Now at the FDA, part of her job is to ensure the safety of medical devices. COVID-19 has carved a new path for Karunasena, as well as other scientists, as they support efforts to review viral detection assays and protective equipment for public safety.
Through her experiences, she remains inspired to help others avoid cancer. The necessity of a proactive approach, she emphasized, is paramount.
-Glenys Young
 News & Notes
News & Notes
Monish Ram Makena, PhD, MS, (’17, ’11) was awarded the 2020 American Association of Cancer Research Breast Cancer Fellowship award and a $120,000 grant for two years to study novel mechanism of resistance in receptor positive breast cancer.
Courtney Queen, PhD, assistant professor in the Julia Jones Matthews Department of Public Health, was selected as a Fulbright U.S. Scholar.
Alok Ranjan, PhD, (’17) joined Virginia Commonwealth University Massey Cancer Center as a research scientist.

Kumari “Iti” Kaushik, MS, graduate student in Pharmaceutical Sciences, received the Syngenta Fellowship Award in Human Health Applications of New Technologies.
 News & Notes
News & Notes
Nursing Graduate: 2019
Stetson Smitherman, BSN, RN, took quite the journey in searching for his dream job. A job where he could help others and make a difference in the world. Teaching, event planning and working for a nonprofit organization were all jobs that Smitherman enjoyed, but none of them really fulfilled his ultimate goal. He had always been inspired by nurses but intimidated by nursing school. Smitherman decided to “take a leap of faith” and attend TTUHSC nursing school where he discovered a career that would achieve his dreams.
 News & Notes
News & NotesMedicine Graduate: 1976
In his 40-year career, John T. Armstrong Jr., MD, has experienced more than 230,000 patient encounters. “I was blessed to have the TTUHSC School of Medicine as my foundation; otherwise, none of this would have happened,” Armstrong said.
He opened his OB-GYN private practice in the Napa Valley after completing his residency at UCSF Medical Center. Armstrong has had some memorable experiences, including delivering a set of quadruplets.

 News & Notes
News & Notes
Graduate: 1985
After treatment for a knee injury she suffered as a high school cheerleader, Cassie Lackey, PT, ATC-r, CPT, knew she wanted to become a physical therapist. Lackey said she should have been able to fully recover from her injury. “Improper exercises and techniques during therapy caused permanent damage to my knee,” she added. Lackey never cheered again and still struggles with knee problems to this day.
 News & Notes
News & NotesPharmacy Graduate: 2009
When COVID-19 caused a hand sanitizer shortage, Brad Martin, PharmD, developed a solution for his community.
The Food and Drug Administration (FDA) gave compounding pharmacies permission to produce alcohol-based sanitizer under a standing order from a local physician to help address the shortage. Initially, Martin contacted a local winery and spirits producer to make ethanol-based sanitizer. However, demand quickly outpaced production.

 Tribute to Founding Faculty Member
Tribute to Founding Faculty Member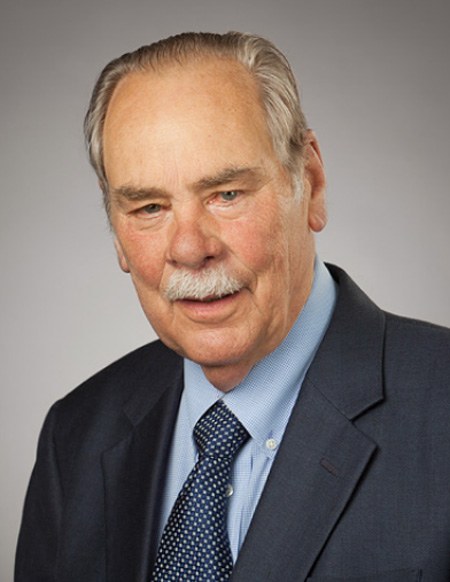
In Room 150 of the Academic Classroom Building, a larger than life portrait of Lorenz “Laurie” Lutherer, MD, PhD, (Medicine ’77) rests next to the lectern. You could almost hear his boisterous laugh as fond memories of him were shared by those who called him colleague, mentor and friend.
Lutherer died Feb. 5, 2020. He joined the School of Medicine in 1972 as a founding faculty member to teach physiology and concurrently pursued his medical degree, with many of his students becoming his classmates. He worked as passionately at developing governance and representation for the faculty as he did in teaching. Luther began a second career at TTUHSC in 2010 as the founding director of the Clinical Research Institute and served as its executive director until his retirement in 2017.



 TTUHSC_SHP
TTUHSC_SHP Texas Tech University Health Sciences Center School of Health Professions
Texas Tech University Health Sciences Center School of Health Professions  @ttuhsc_shp
@ttuhsc_shp